 |
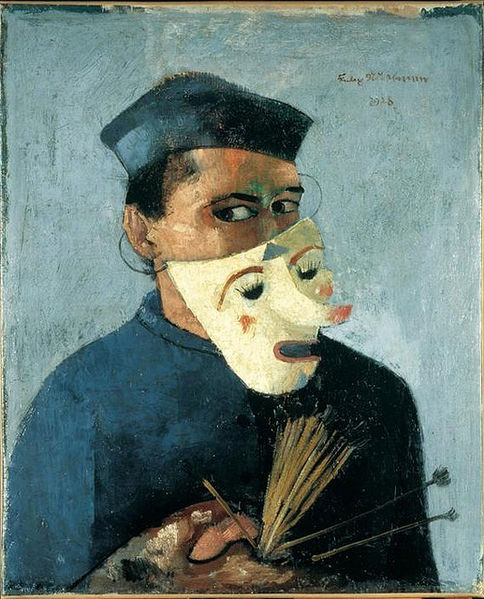
A glimpse of the SP under the patient mask.
[Self-portrait with Mask via wikimedia] |
When learners feel particularly self-conscious in a scenario, they often break character. This could be because the scenario is new, they're not confident in their abilities, or because a subject is particularly uncomfortable (e.g.: sexual history).
When a learner breaks character, they may talk to themselves, ask the SP a direct question rather than the patient, or make a guess about what they think is supposed to happen in the scenario. It is often accompanied by an expression of appeal towards the SP to get the SP to break character, too. Sometimes they smile to indicate they're in on the joke. I think learners do this because it gives them some control & power in a situation where they feel insecure.
As an SP, it takes a tremendous amount of will to resist or deflect this. So if a learner asks me a direct question like, "So am I supposed to examine your heart?," I have to react like a patient: "I don't know? I guess? I mean, you're the doctor, ha ha!" Or I have to keep a straight face while the learner is clearly looking for more information but hasn't asked for it yet.
Sometimes that's enough pushback for the learner to realize they really do have to pretend to be a medical professional for this encounter. And so we move on.
Sometimes it's not, though. A scenario is a fascinating place that only works when everyone involved agrees to create a shared fantasy. If one person isn't into it, the whole thing limps along until time is called.
That can lead to awkward feedback. In a scenario like that, if I try to give feedback about what I observed, the learner is often defensive. So instead I try to talk with them about why the s/he had trouble taking the encounter seriously. Sometimes we talk about the purpose of scenarios. Even if it doesn't feel real to
them, it feels real to
me. So the more seriously they treat the encounter, the better feedback I can give.