|
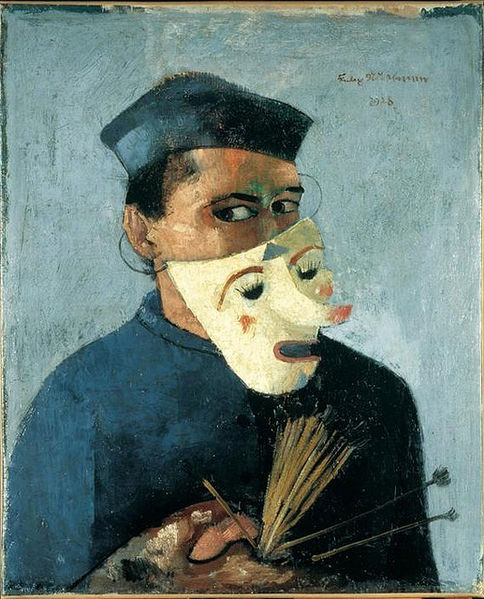
| Calliope, the muse of epic poetry, approves this post. [La Muse Calliope via wikimedia] |
This post original began as simply a grateful reference to Empathy 101 (how to sound like you give a damn), because I give similar feedback to learners. I nodded deeply in agreement when I read:
- "Reassurance often fails if the physician does not also communicate an awareness of the patient’s deepest fears or concerns."
- "This model of doctor-patient communication begins with empathic listening and responding, requires reflectivity and self-understanding, and is in itself a healing act."
- The list of "Statements That Facilitate Empathy," which is a particularly useful tool.
But then I realized these quotes and tools are all by the same person, which is how I discovered Dr. Jack Coulehan. Coulehan has written both "Let Me See If I Have This Right… – Words That Help Build Empathy" for the Annals of Internal Medicine as well as the textbook Metaphor and Medicine: Narrative In Clinical Practice.
Sadly, neither of those references appear to be available via my normal channels, but some of his other books are, and that's how I learned Coulehan is both a doctor and a poet!
For instance, in addition to his own poetry, Coulehan edited Chekhov's Doctors: A Collection of Chekohov's Medical Tales as part of the Literature and Medicine series. Perfect for actors, eh? The Kindle edition has a much more interesting description of it: "In his brief but distinguished life, Anton Chekhov was a doctor, a documentary essayist, an admired dramatist, and a humanitarian. He remains a nineteenth-century Russian literary giant whose prose continues to offer moral insight and to resonate with readers across the world. Chekhov experienced no conflict between art and science or art and medicine. He believed that knowledge of one complemented the other. Chekhov brought medical knowledge and sensitivity to his creative writing—he had an intimate knowledge of the world of medicine and the skills of doctoring, and he utilized this information in his approach to his characters. His sensibility as a medical insider gave special poignancy to his physician characters. The doctors in his engaging tales demonstrate a wide spectrum of behavior, personality, and character. At their best, they demonstrate courage, altruism, and tenderness, qualities that lie at the heart of good medical practice. At their worst, they display insensitivity and incompetency. The stories in Chekhov's Doctors are powerful portraits of doctors in their everyday lives, struggling with their own personal problems as well as trying to serve their patients. The fifth volume in the acclaimed Literature and Medicine Series, Chekhov's Doctors will serve as a rich text for professional health care educators as well as for general readers."
The intersection of art & science is one of my very favorite things. Looking forward to reading more work by Jack Coulehan.